By Emma McShane, Dietitian, August 2021
What is Mastitis?
Mastitis is inflammation of the breast tissue, affecting 10-25% of breastfeeding women. The majority of cases occur during the first 6 weeks of breastfeeding, however mastitis can occur at any time during the breastfeeding journey. Mastitis can be caused by engorgement or inadequate milk removal from the breast, resulting in a blocked duct. This causes the milk blocked behind the duct to be forced into the nearby breast tissue, causing inflammation. This inflammation is known as mastitis and can lead to infection. Fast and supportive treatment is needed, as mastitis can lead to early weaning from the breast, or complications such as a breast abscess if left untreated.
Mastitis may occur due to latching problems, sucking issues, sleepy babies, oversupply, or hurried feeds, including limiting a baby’s time at the breast. These factors can affect how much milk is drained from the breast.
How do I prevent Mastitis?
- Ensure your baby is well-positioned and attached to the breast.
- Make sure your bra is loose and there is no pressure on your breasts e.g. clothing or fingers while feeding.
- Feed on demand, offering flexible and frequent access to the breast, as missed feeds or long intervals between breastfeeding can increase your risk of developing mastitis.
- Relax whilst breastfeeding to help encourage your milk flow.
- Gently massage the breast by stroking towards the nipple whilst your baby feeds.
- If your breasts become uncomfortably full, wake up your baby to feed them. If they do not want to feed, express a small amount for comfort.
- Hand express to empty the breast.
- Practice good hygiene, and if using a breast pump, clean this often, as this will help to prevent contamination.
- Check your breasts frequently for lumps, pain, or redness.
- Alternate from which breast you begin each feed, as this will help to ensure one breast is drained well at every second feed.
- Let your baby finish when they’re ready to ensure they have taken the most milk out of the breast. Avoid timing your baby at the breast.
- If you choose to wean your baby, make sure you do this slowly as rapid weaning can cause mastitis.
- Stress, fatigue, vigorous exercise, or overall poor health and nutrition can increase your risk of mastitis, so self-care and adequate nutrition is essential.
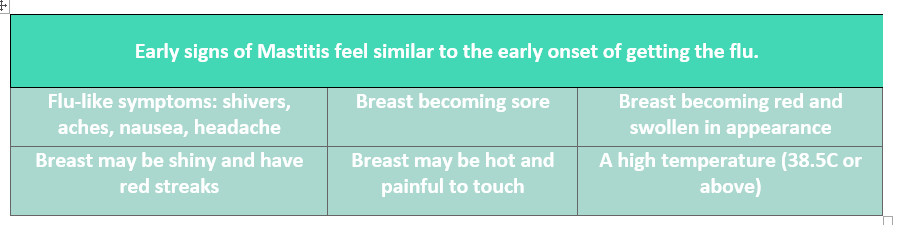
Symptoms:
Please note that some mothers do not get the early signs of a blocked duct, and feel that mastitis comes on ‘out of the blue’.
Treatment:
It is important that if you feel a blocked duct coming on, to start treatment immediately. The most important part of treatment is to allow for effective milk removal, regularly.
- It is important to drain the breast often, but gently.
- Feed frequently, starting on the affected breast. This is not the time to wean your baby as symptoms can worsen. Allow your baby to drain the breast and also make sure that you are offering the unaffected breast. The milk is safe for your baby to drink.
- Change feeding positions as this may help to clear the blockage. You can try positioning your baby at the breast with their chin or nose pointing to the blockage, as this will help drain the affected area.
- Gently massage your affected breast, as this will help to improve drainage and symptoms.
- Ensure good positioning and latch. A lactation consultant can help you to achieve this.
- Use cold packs on the affected breast, as this can help to reduce swelling and relieve pain.
- Use warm heat packs sparingly just before bed (only for a few minutes), to help trigger your let-down to help clear the blockage.
- It is very important to get as much rest as possible.
- Simple analgesia can be taken as needed such as paracetamol or ibuprofen.
- When treated promptly, a blocked duct should clear in 24-48 hours.
- If the blockage is not clearing within 24 hours, seek advice from your doctor, as antibiotics may be needed if an infection occurs. Please note that antibiotics only treat an infection, not the cause of the blockage.
- Milk supply can sometimes be affected when mastitis is occurring, so look out for signs that your baby is getting enough milk including urine and stool output, and that your baby is putting on weight. A change in supply can be addressed with frequent and effective feeding.
- A Lactation Consultant can check your baby’s positioning at the breast to prevent mastitis & blocked ducts.
- Breast ultrasound can be an adjunct to treatment to help clear the blocked duct.
Nutrition:
It is very important to keep up your fluids, which means consuming >2 litres per day
- Breastfeeding is a demanding process on the body that requires more energy and protein than usual. Other important nutrients include iron, iodine, and calcium. A dietitian can help you to meet your requirements.
- Try to eat regular meals & snacks across the day, even if feeling unwell.
- Simple meal and snack ideas include: Scrambled eggs with toast and chopped vegetables, baked beans on toast, roasted chickpeas, vegetable sticks and hummus or cheese and crackers.
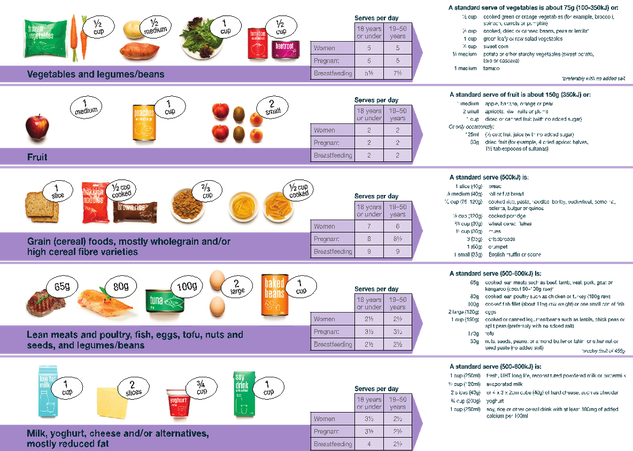
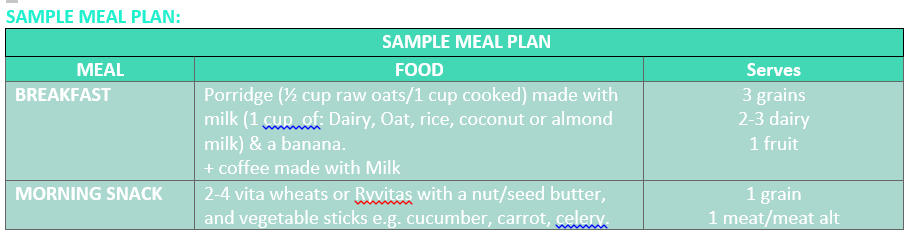
- Below is the Australian Guide to Healthy Eating recommended serves for each food group during breastfeeding.
Are probiotics helpful?
- Scientific trials have found inconclusive results on the benefits of probiotics to prevent or treat mastitis. There is an emerging field of research to suggest that probiotic use may help to prevent mastitis, however further research needs to be conducted in this area to reach a conclusion.